Although human seminal fluid contains melatonin and spermatozoa reportedly possess membrane melatonin receptors, there are no experimental studies that have ascertained the relationship between melatonin and male infertility.
This study evaluated whether urinary 6-sulfatoxymelatonin and urinary total antioxidant capacity correlate with different seminal parameters including sperm concentration, motility and morphology. Also, the in vitro effects of melatonin on human sperm motility were investigated.
Semen samples from 52 men who were counselled for infertility were obtained. Sperm concentration was determined using the haemocytometer method, motility kinematic parameters were assessed using a computer-aided semen analysis system, while morphology and vitality were evaluated after Diff-Quick and Eosin-Nigrosin vital staining, respectively. For the quantification of urinary 6-sulfatoxymelatonin, a commercial ELISA kit was used, and urinary total antioxidant capacity was evaluated by means of a colorimetric assay kit.
For the in vitro effects of melatonin, samples were incubated for 30min in the presence or absence of 1mm melatonin. Both urinary 6-sulfatoxymelatonin and total antioxidant capacity levels positively correlated with sperm concentration, motility and morphology, as well as negatively correlated with the number of round cells. Additionally, 30-min exposure of sperm to 1mm melatonin improved the percentage of motile and progressively motile cells and decreased the number of static cells, thereby promoting the proportion of rapid cells.
Therefore, melatonin improves semen quality, which is important because melatonin supplementation may be potentially used to obtain a successful assisted reproductive technique outcome.
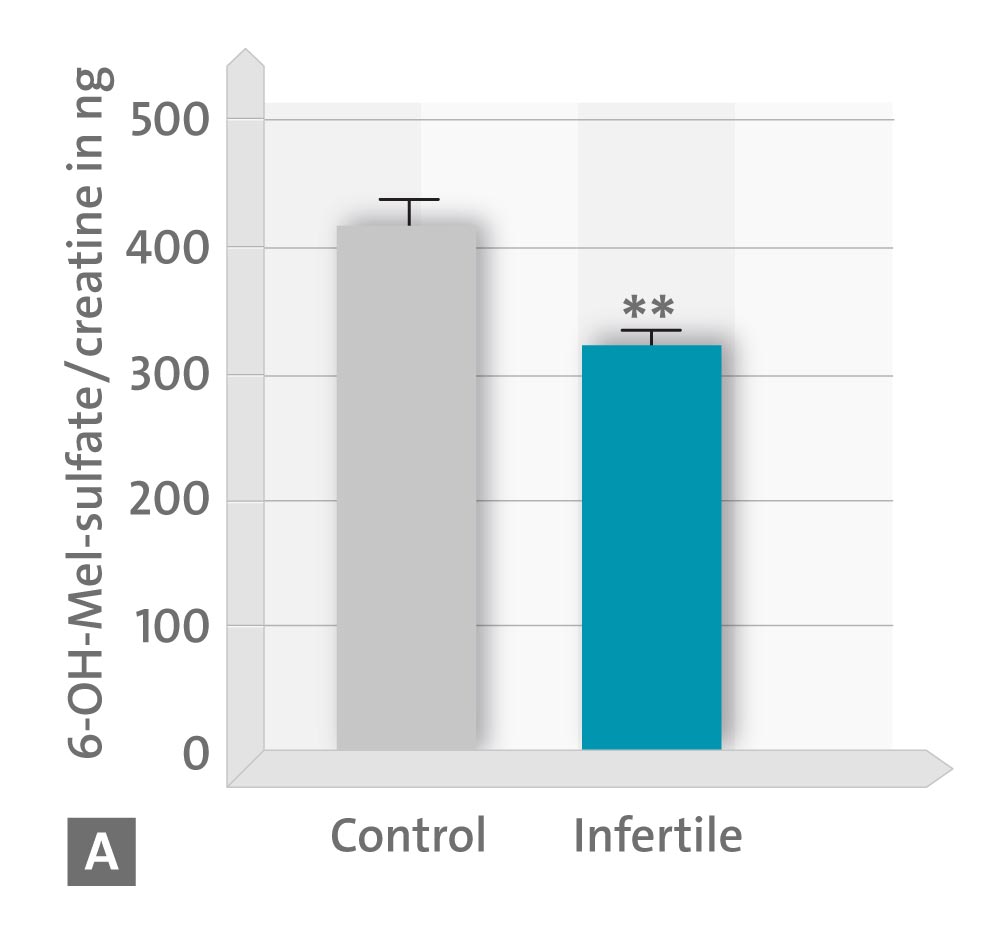
• A concentration of 6-hydroxymelatonin sulphate (6-OHMS) in urea;
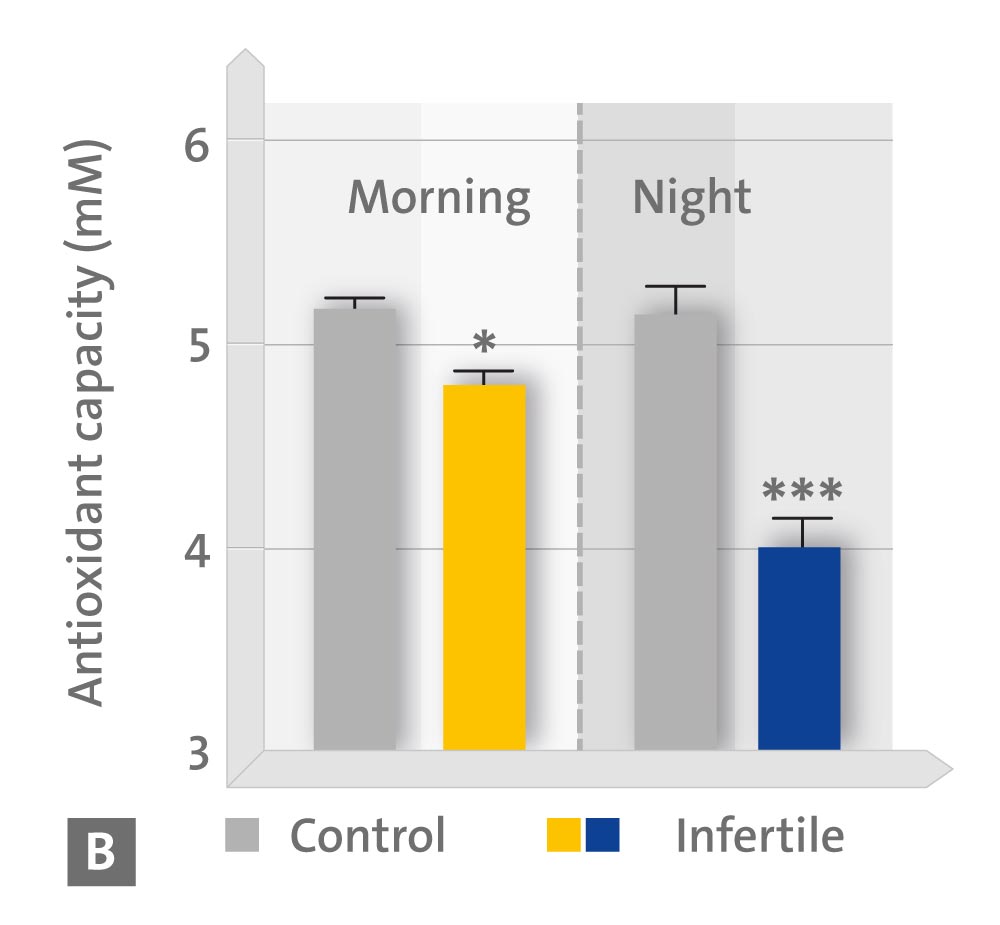
• B day and night values of the anti-oxidative capacity in the urea;
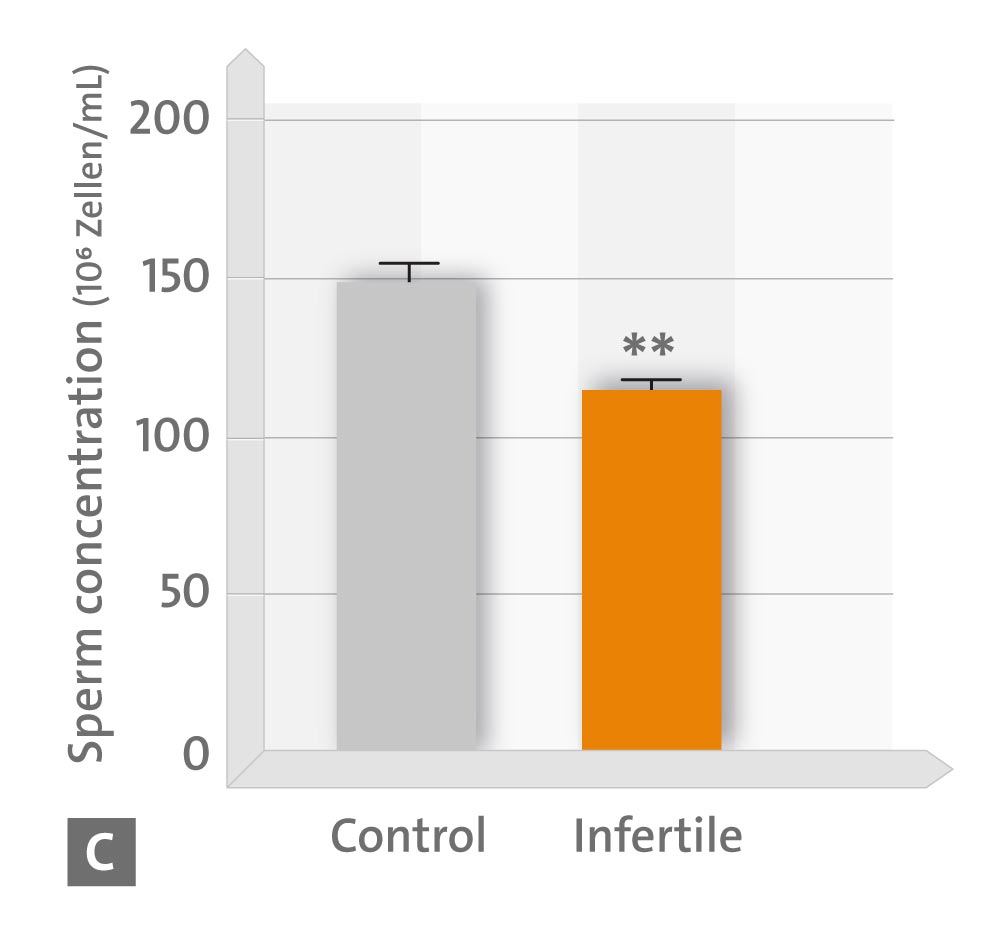
• C sperm concentration,
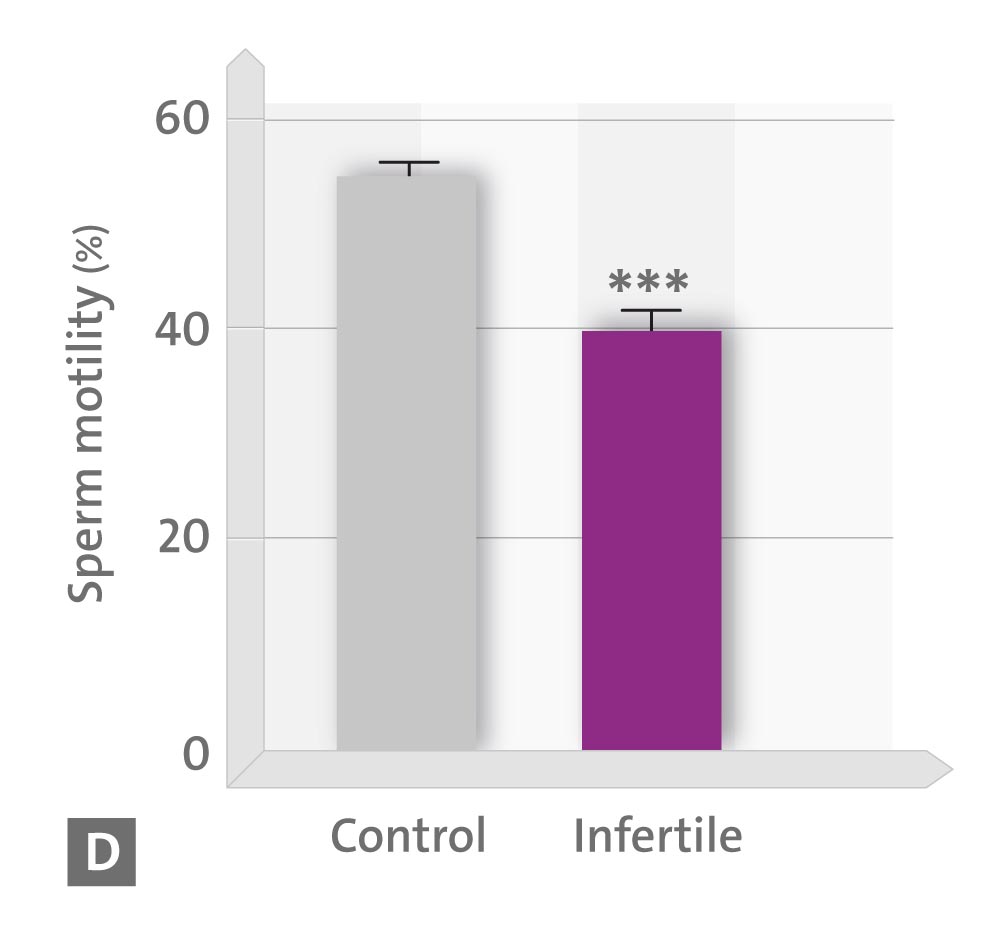
• D sperm motility,
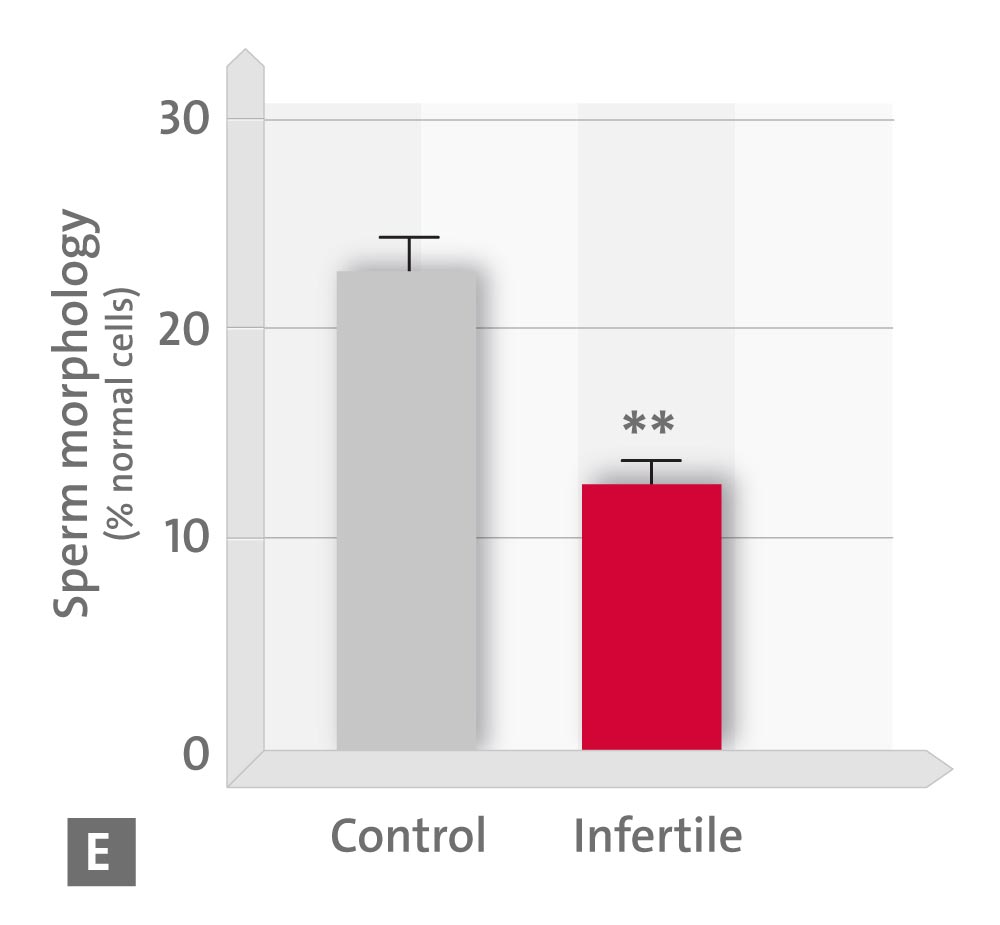
• E sperm morphology and
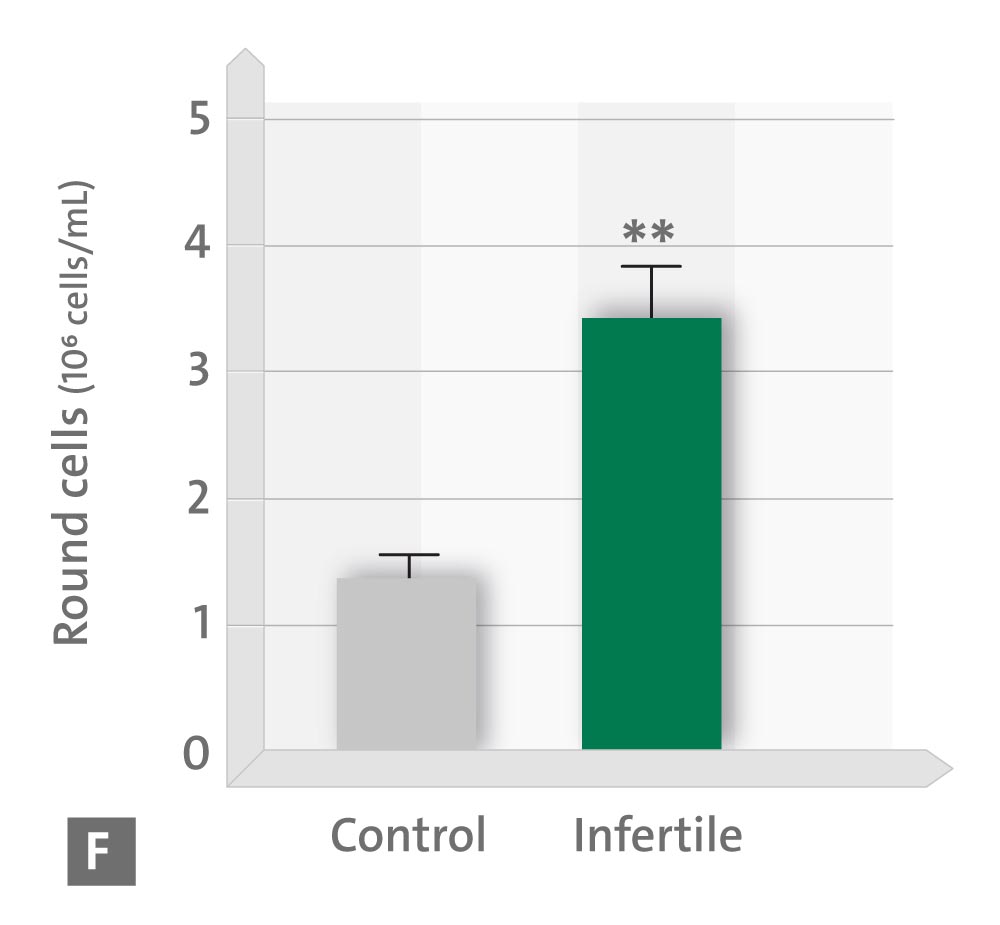
• F number of the round sperm cells in the ejaculate.
* p < 0.05; ** p < 0.01; *** p < 0.001 vs. controls (Source: modified according to Ortiz A et al., 2011)